Body Mass Index (BMI) has been relied on as a convenient measure to diagnose underweight, overweight and obesity. The cut-offs for overweight and obesity are routinely used to determine disease risk and even eligibility for surgery. However, the availability of new data is now leading some specialists to question the traditional reliance on BMI. A publication in PLOS ONE last month (Visaria A et al) showed results of a study including over 554,000 adults. The risk of all-cause mortality across a range of BMI categories (22.5 – 24.9 kg/m2; 25.0 – 27.4kg/m2; 27.5 – 29.9kg/m2), including groups conventionally considered overweight was similar.
Focusing on adolescent obesity, a Viewpoint published in JAMA challenges guidelines from the American Academy of Pediatrics (AAP). Skolink notes findings which are at odds with the conventional link between BMI and health outcomes:
• 60% of adolescent athletes who are obese based on BMI do not meet the definition using skinfold thickness.
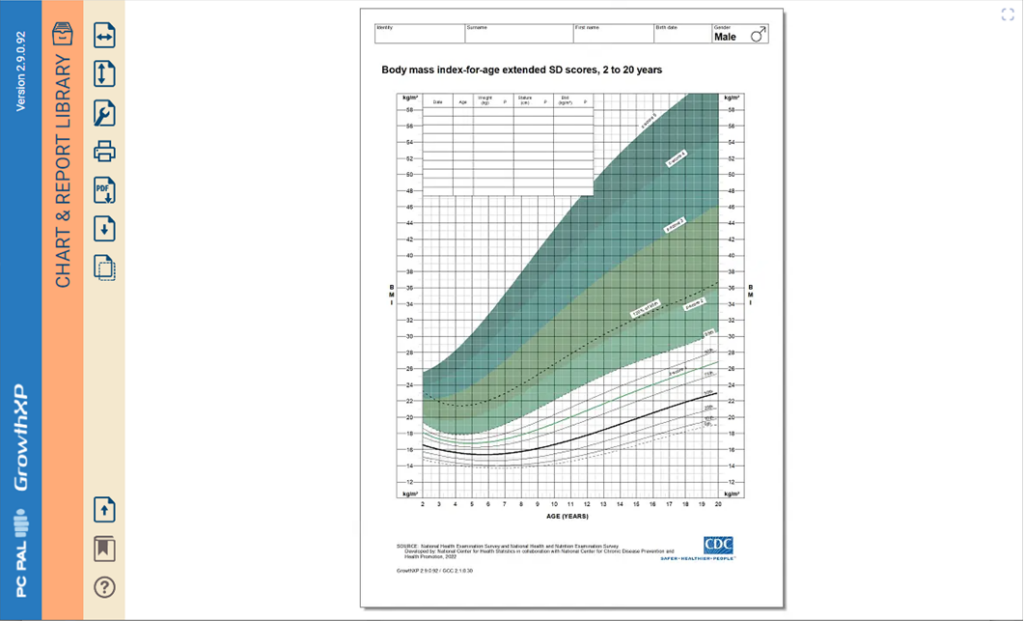
• 30% of adolescents obese according to their BMI are not obese at age 30. Other measures of body composition, which are also convenient in clinical practice are available including skinfold thickness, waist circumference and waist-hip ratio. Skinfold thickness is included within the childhood growth monitoring application, GrowthXP, in addition to visualisation of BMI.
References:
Visaria A et al. PLoS ONE 18(7): e0287218. https://doi. org/10.1371/journal.pone.0287218
Skolnik N. The American Academy of Pediatrics Obesity Guidelines—A Critical Appraisal. JAMA Pediatr. 2023;177(8):747–748. doi:10.1001/jamapediatrics.2023.1577)